Septoplasty, or septal reconstruction, surgery is largely considered a functional, or medically necessary, procedure intended to help straighten a deviated septum, or crooked septum. Many patients have at one time or another heard of friends or family members who have been diagnosed with a deviated septum.
What Exactly Is The Septum?
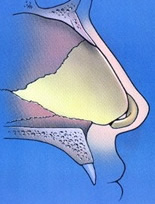
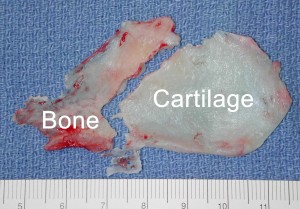
Simply put, the septum is the wall that divides the left and right sides of the nose internally. If you look into the nostril opening with a light, you should see a vertical structure, or wall, that physically divides the left and right sides starting from just behind the columella (the fleshy column of skin that separates the two nostrils). The septum extends from just behind the columella going backward into the nose and stops at the nasopharynx (the common cavity in the extreme back of the nose, which communicates below into the back of the mouth). The septum is naturally a three layered structure that is almost like a sandwich turned vertically. There is a mucosal lining on each side that would be the bread. In between the two mucosal linings in the middle is the cartilage and bone of the septum. A majority of the septum is made of cartilage, which comprises the anterior 2/3 of the entire septum. The adjacent diagram is a side view of the inside of the nose showing the septum from the nostrils all the way back as it approaches the nasopharynx. In the diagram, the cartilage is represented by the yellow shaded area and the bone by the gray shaded area. The bone is divided into two segments – the upper a portion from the ethmoid bone and the lower termed the vomer. What does this look like in real life? The adjacent photo demonstrates what the actual bone and cartilage look like from a patient who had nasal surgery where the bone and cartilage were explanted temporarily. It is a great visual showing the bone of the septum on the left side and the cartilage on the right. This amount of cartilage and bone is not actually removed in standard septoplasty surgery. It is simply shown for demonstration purposes only.
What Is A Deviated Septum?
A deviated septum is simply one that is crooked to one side and/or the other and obstructs the nasal passageway used for breathing. In most patients, a deviated septum is congenital, meaning they were born with the abnormality. At some later date, they begin to notice some difficulty breathing through the nose from one or both sides. Usually this is appreciated as someone begins to exercise more regularly and notices a significant difference in airflow between the two sides. In other cases, the deviated septum becomes apparent during evaluation for other medical conditions, such as sinus inflammation (sinusitis) or allergies. In other patients, a traumatic injury to the nose can cause a shift in the positioning of the septum, resulting in a deviation that causes nasal obstruction symptoms. Normally the septum is oriented in a relatively straight line as it goes back into the nose. In situations where a deviation exists, the septum can be curved, crooked or displaced to one or both sides. The deviation usually involves mostly cartilage but can involve both cartilage and bone in some circumstances. When the septal cartilage and bone deviate from the middle, the normal airflow through the nose can be disrupted. When this occurs, patients subjectively feel as if they are unable to breathe sufficiently through one or both sides of their nose. If this happens in the setting of other medical conditions, like sinusitis and allergies, the deviated septum can make matters worse.
Diagnosis Of A Deviated Septum

The diagnosis of a deviated septum is best done through a physical examination performed by a qualified nasal specialist – either a board certified otolaryngologist (ENT surgeon) or a board certified facial plastic surgeon. On physical examination, your doctor will use what is called a nasal speculum to prop open your nostril on each side as a light is used to visually inspect the nasal passageway.A septal deviation will be seen as a curvature or displacement of the septum into the nasal passageway. The adjacent photo of one of my San Diego septoplasty patients shows this visually. As you can easily appreciate, there is a significant curvature of this patient’s septum into their left nasal passage causing a rather obvious blockage. In fact, you can see a very narrow vertical slit of darkness in the left nasal passage, corresponding to the only area where airflow can get through this particular patient’s nose. Although a deviated septum is typically easily diagnosed on physical examination, some patients end up getting a CT (CAT) scan of their nose as part of the diagnostic evaluation. In my opinion, this is usually not necessary. However, many insurance companies require that a CT scan be done in order to objectively confirm the existence of a septal deviation.
What Is A Septoplasty?
Septoplasty, or septal reconstruction, is a surgical treatment for a deviated septum. The surgery is usually performed thru the nostrils without having to make any external incisions on the nose. In short, the mucosal lining covering the septum is elevated, or lifted, off of the cartilage and bone. It is actually lifted off of both sides in order to fully expose the deviated segments of cartilage and bone. The deviated portions of the septum are then carefully trimmed and removed in most cases. 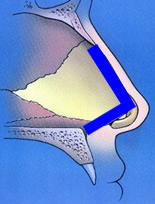 Septoplasty surgeons have to be very careful, however, to preserve what is termed the L-strut of the septum whenever they are performing surgery. The L-strut is represented by the blue L-shaped figure in the adjacent diagram. As you can see, the long portion of the L-strut provides support for the nasal bridge and the short portion of the L-strut provides support for the nasal tip. It is critical that a sufficiently strong L-strut is preserved during septoplasty. If not, the support of the nasal bridge and tip can be significantly compromised, resulting in collapse of the nose. As long as an adequate L-strut is preserved in septoplasty, you can feasibly remove the deviated portions of the septum with relative impunity without changing the cosmetic appearance of the nose. In fact, in standard cases of septoplasty there should be no change in the appearance of the nose.
Septoplasty surgeons have to be very careful, however, to preserve what is termed the L-strut of the septum whenever they are performing surgery. The L-strut is represented by the blue L-shaped figure in the adjacent diagram. As you can see, the long portion of the L-strut provides support for the nasal bridge and the short portion of the L-strut provides support for the nasal tip. It is critical that a sufficiently strong L-strut is preserved during septoplasty. If not, the support of the nasal bridge and tip can be significantly compromised, resulting in collapse of the nose. As long as an adequate L-strut is preserved in septoplasty, you can feasibly remove the deviated portions of the septum with relative impunity without changing the cosmetic appearance of the nose. In fact, in standard cases of septoplasty there should be no change in the appearance of the nose.
Many surgeons will say they simply ‘score’ the septal cartilage and thereby weaken it, instead of actually removing the deviated segment. Scoring the cartilage means they make partial cuts into the cartilage using a scalpel with the cuts made only on one side of the deviation. This can help straighten the curved portion of cartilage. On the operating room table, the cartilage does, indeed, appear much straighter from the scoring process. Unfortunately, cartilage has what is called ‘memory’ – meaning it wants to go back to its original shape if left intact. In cases where scoring is performed over a deviation, the cartilage will often times simply bend back to its crooked position once the healing process takes place. This is why some patients (and surgeons) mistakenly say their septum ‘grew back’ after a prior septoplasty. In fact, what happened is that the septal memory kicked in and resulted in the deviation returning to its original position (along with recurrent symptoms of nasal obstruction). It is for this reason that most experienced septoplasty surgeons will remove the deviated portions of cartilage and not rely on scoring as a reliable method of straightening the nasal airway. In some cases, portions of the septal bone in the back of the nose also need to be addressed. In these patients, the bone can be cut with specialized surgical instruments to strategically remove the deviated segments. Once the cartilage and bone are straightened out, the mucosal lining on each side is redraped, or put back into position. The mucosal lining is the sewn together using a specially designed needle just for this purpose. The suture thread used to sew the lining together is absorbable – usually dissolving within 10-14 days following the surgery.
Do You Pack The Nose Following Septoplasty?
I actually do not pack the nose routinely following septoplasty, or septal reconstruction. Many septoplasty surgeons use packing to help hold the lining together following surgery. Others will place a splint inside of the nose along each side of the septum to hold things in place during the early healing process. Unfortunately, packing and splints can both be quite uncomfortable. In fact, the packing and splints can account for a majority of pain and discomfort following routine septoplasty surgery. Because of this reason, I normally rely on my internal suture technique to carefully sew the lining back together in a fairly complete fashion. In doing so, this precludes me from having to place packing in the nose. In cases where there is slightly more bleeding than anticipated, I might put an absorbable material inside the nose to help control unwanted bleeding. But, fortunately, this material dissolves on its own with use of saline sprays inside of the nose and does not have to be removed.
How Long Is The Recovery After Septoplasty?
Most patients undergoing septoplasty surgery will have a downtime of around 5-10 days. The recovery is mainly limited by mild discomfort, which is fairly well controlled with low dose narcotic pain medication such as Vicodin or Tylenol with codeine. As noted above, there is no change to the appearance of the nose with standard septoplasty, you should not notice any external swelling or bruising. Because of this, most patients feel quite comfortable in the public eye fairly soon after surgery.
Does Health Insurance Cover Septoplasty Surgery?
In most cases where there is a deviation of the septum and the patient has trouble breathing through the nose as a result of this, health insurance should cover you to have the septoplasty performed. Many insurance companies like to see that you have been tried on other medical treatments (such as topical nasal steroids) before they consider you a candidate to undergo a septoplasty. Although the medications will not do anything to correct your deviated septum, some medications might help open up your nasal passages in other ways to at least allow some degree of improvement. The thought is that this might provide you sufficient relief that surgery may not be needed after all. It is my recommendation that you consult with a board certified otolaryngologist (ENT surgeon) or board certified facial plastic surgeon in your area to determine whether or not you are a candidate for septoplasty. To learn more about insurance coverage for nasal surgery, use this link to be taken to our online tutorial.